楚楚 发表于 2012-10-22 16:45
由于该事件是由于成品药污染所致的感染暴发事件,所以我们会习惯性认为与我们的医院感染工作无关。icchina说 ...
该事件的后续报道?
甲泼尼龙注射导致真菌感染的临床发现
英文原标题: Clinical findings for fungal infections caused by methylprednisolone injections.
作者:Tom M Chiller ,Monika Roy ,Duc Nguyen ,Alice Guh ,Anurag N Malani ,Robert Latham
期刊名称:新英格兰医学杂志(NEJM)
发表时间:2013-10-24
索引:N. Engl. J. Med..2013 Oct 24;369(17):1610-9.
中文摘要来源:麦毓麟翻译
中文摘要
研究背景:
从2012年9月18日开始,公共卫生官员一直在调查一宗大型真菌性脑膜炎及其他感染的暴发,这些病人都接受过感染后乙酸甲泼尼龙的硬膜外、脊椎旁或关节内注射。我们对于本次感染的病原体嘴突脐孢了解很少。本研究旨在描述本次暴发相关感染的早期临床病程。
研究方法:
我们对2012年11月19日前报道给疾病控制及预防中心的爆发案例的医疗记录进行回顾,这些病例来自报道案例最多的六个州(佛罗里达州、印第安纳州、密歇根州、新泽西州、田纳西州和维吉尼亚州)。我们使用聚合酶链式反应和免疫组化测试对临床分离物及组织样本进行病原学确认。
研究结果:
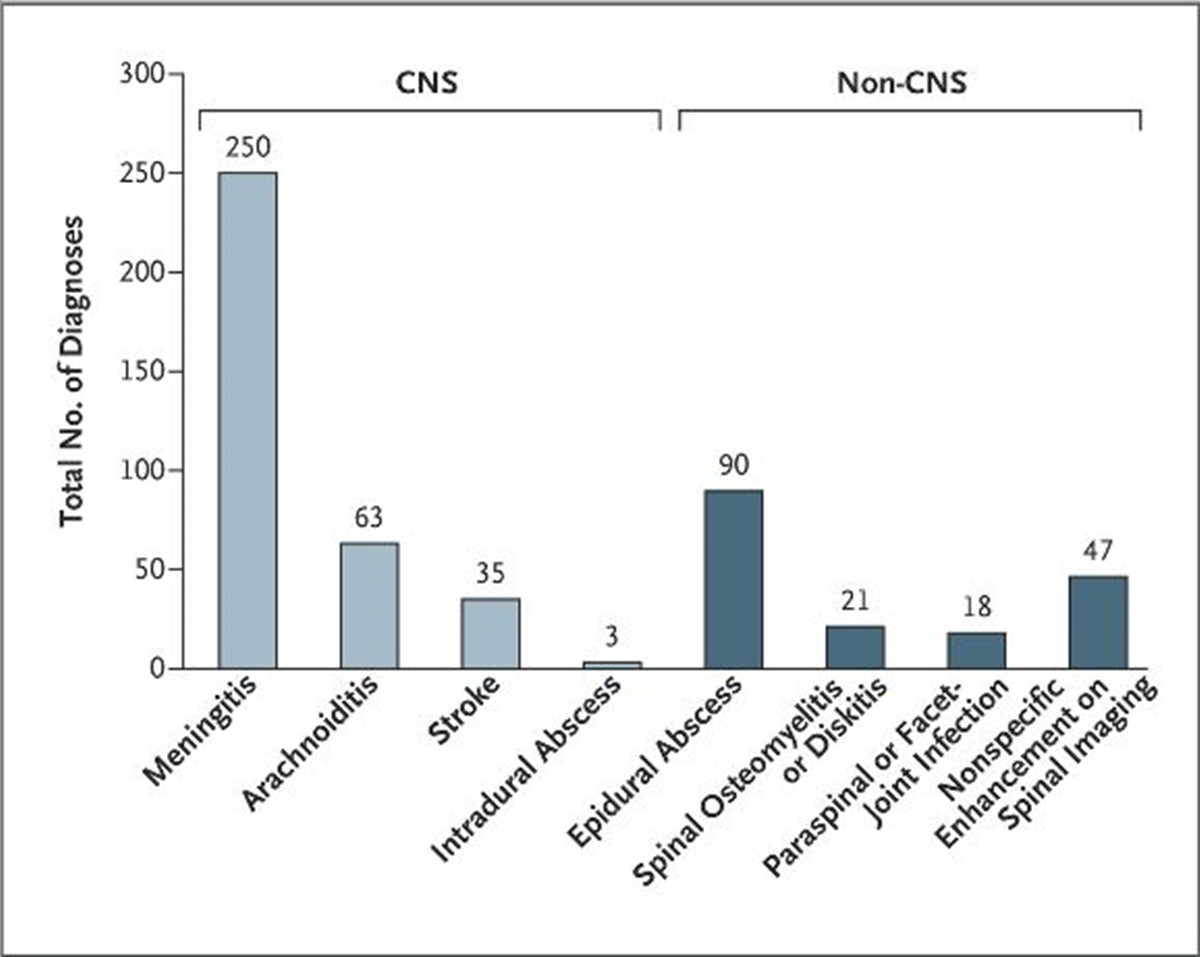
本次研究共入组了无外周关节感染的328名患者,265名(81%)存在中枢神经系统(CNS)感染,63名(19%)只存在非CNS感染。268名能获得样本的患者中,96名找到了嘴突脐孢感染的实验室证据。对于存在CNS感染的患者中,卒中的发生与脑脊液中异常指标的严重增加相关(P<0.001)。爆发的后期出现非CNS感染更频繁(从末次注射到诊断的中位间隔时间,硬膜外脓肿为39天,卒中为21天;P<0.001),同时无论患者有无脑膜炎,这类感染都会发生。
研究结论:
本次爆发的初始临床发现提示硬膜外和脊椎旁注射污染糖皮质激素产品导致的真菌感染会造成一系列的临床疾病,反映了致病机制、宿主及暴露风险因素可能出现的变异。
英文摘要
BACKGROUND
Since September 18, 2012, public health officials have been investigating a large outbreak of fungal meningitis and other infections in patients who received epidural, paraspinal, or joint injections with contaminated lots of methylprednisolone acetate. Little is known about infections caused by Exserohilum rostratum, the predominant outbreak-associated pathogen. We describe the early clinical course of outbreak-associated infections.
METHODS
We reviewed medical records for outbreak cases reported to the Centers for Disease Control and Prevention before November 19, 2012, from the six states with the most reported cases (Florida, Indiana, Michigan, New Jersey, Tennessee, and Virginia). Polymerase-chain-reaction assays and immunohistochemical testing were performed on clinical isolates and tissue specimens for pathogen identification.
RESULTS
Of 328 patients without peripheral-joint infection who were included in this investigation, 265 (81%) had central nervous system (CNS) infection and 63 (19%) had non-CNS infections only. Laboratory evidence of E. rostratum was found in 96 of 268 patients (36%) for whom samples were available. Among patients with CNS infections, strokes were associated with an increased severity of abnormalities in cerebrospinal fluid (P<0.001). Non-CNS infections were more frequent later in the course of the outbreak (median interval from last injection to diagnosis, 39 days for epidural abscess and 21 days for stroke; P<0.001), and such infections developed in patients with and in those without meningitis.
CONCLUSIONS
The initial clinical findings from this outbreak suggest that fungal infections caused by epidural and paraspinal injection of a contaminated glucocorticoid product can result in a broad spectrum of clinical disease, reflecting possible variations in the pathogenic mechanism and in host and exposure risk factors. (Funded by the Centers for Disease Control and Prevention.).
相关图片
相关资料 |